Many people carry invisible wounds. Trauma doesn’t always announce itself—it hides in emotional triggers, symptoms of anxiety or depression, and even struggles with addiction.
Research shows that adverse childhood experiences (ACEs) are common, affecting nearly two-thirds of adults. For those seeking healing, trauma-informed care offers a compassionate, empowering path forward by prioritizing safety and trust.
Trauma-informed care is a compassionate approach to health care that prioritizes emotional safety, trust, and empowerment—especially for those with a history of trauma.
By understanding the impact of trauma, this method reshapes care services to avoid re-traumatization and encourage healing. Through trauma-informed care training, providers can better meet individuals where they are, offering support rooted in empathy, choice, and collaboration.
What Is Trauma-Informed Care?
Trauma-informed care is a compassionate approach that recognizes the wide effects of trauma and prioritizes safety, trust, and empowerment throughout healing.
This care model understands that trauma—whether a single event or ongoing stress—shapes how people experience mental health services, relationships, and treatment. Trauma-informed practices aim to prevent retraumatization and help individuals feel safe, respected, and in control.
Key principles guide trauma-informed care to create safe, supportive, and empowering environments:
- Safety: Physical and emotional safety for patients and staff is essential.
- Trustworthiness and Transparency: Clear communication builds trust and prevents misunderstandings.
- Peer Support: Those with trauma experience offer unique, empowering support.
- Collaboration and Mutuality: Healing works best when power is shared between providers and clients.
- Empowerment, Voice, and Choice: People are supported in making decisions and rebuilding confidence.
- Cultural, Historical, and Gender Sensitivity: Respecting identity and background ensures inclusive care.
Unlike traditional models focusing just on symptoms, trauma-informed care shifts the question from “What’s wrong with you?” to “What happened to you?”.
Training helps professionals recognize trauma responses and tailor care to the person—not just the diagnosis.
Why Does Trauma-Informed Care Matter?
Trauma-informed care creates a safe space for healing by reducing retraumatization and building trust.
Many people entering treatment—especially for substance abuse and mental health concerns like PTSD, anxiety, or depression—have a history of trauma. These traumatic events may include childhood abuse, neglect, violence, or prolonged stress. When care providers don’t recognize these experiences, treatment can unintentionally trigger fear, shame, or resistance.
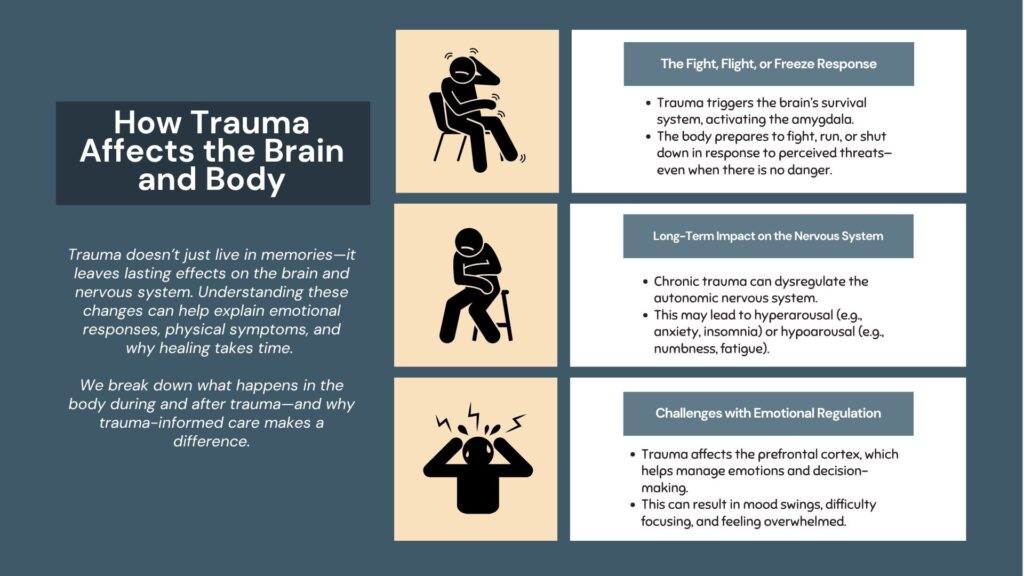
That’s where trauma-informed care makes a powerful difference. This approach understands the deep impact of trauma and how it shapes a person’s emotional and physical responses. Instead of focusing solely on symptoms, trauma-informed care honors each person’s story—including adverse childhood experiences (ACEs)—and treats the whole person with compassion.
By creating emotionally safe, empowering environments, trauma-informed care helps individuals rebuild trust, regain a sense of control, and move toward lasting healing. It acknowledges the effects of trauma while offering a path forward rooted in choice, voice, and dignity. This model doesn’t just help patients—it also improves outcomes and relationships between patients and staff, making care services more effective, inclusive, and humane.
Common Questions And Misunderstandings
It’s normal to have questions or concerns when exploring trauma-informed care. Many people feel uncertain or confused, especially if they’re just starting to understand the impact of trauma. The answers below can help clarify what trauma-informed care really means—and why it matters.
How is trauma therapy different from regular therapy?
Trauma therapy uses trauma-informed care principles to create a safe, empowering space for healing. Instead of focusing only on symptoms, it considers the effects of trauma on the nervous system, emotional patterns, and sense of safety.
A trauma-informed therapist will prioritize emotional regulation, trust-building, and collaboration. You won’t be pressured to “push through” difficult topics. Instead, care is paced and respectful of your comfort. This approach helps people feel more supported—especially those recovering from a traumatic event, abuse situation, or long-term substance abuse and mental health challenges.
How do you deal with trauma you don’t remember?
You don’t need to remember everything to heal. Many people have gaps in memory due to the brain’s response to trauma. These gaps are normal. Trauma-informed care focuses on present-day experiences, emotional responses, and behavioral patterns—not on forcing memories. Whether the trauma is clear or vague, healing can still happen.
Informed care meets you where you are. It focuses on helping you feel safe, develop coping tools, and gently explore how past experiences may shape current challenges.
“You have to relive your trauma to heal.”
This is a common myth—and it’s not true. Trauma-informed care does not require you to relive or retell painful events in detail. In fact, doing so without proper support can be retraumatizing. Instead, providers trained in trauma-informed care practices offer consent-based care, where you’re always in control of what you share and when.
Healing comes through choice, trust, and building emotional resilience—not through forced exposure to pain.
“If you don’t remember the trauma, it doesn’t affect you.”
Even if you don’t consciously remember the trauma, it can still have an impact. This includes adverse childhood experiences (ACEs) and early abuse and mental health challenges that shape how the brain and body respond to stress.
Symptoms like anxiety, hypervigilance, low self-worth, or trust issues may all point to experienced trauma, even if the cause isn’t fully remembered.
A trauma-informed approach respects this complexity. It helps individuals heal without requiring detailed recollection—because your body and mind may already be telling the story.
How Does Trauma-Informed Care Work?
Trauma-informed care is a thoughtful approach used in clinical settings to create safety and support healing. Care teams are specially trained to recognize trauma and respond with kindness and respect.
Some key practices, or trauma informed care examples, include:
- Active listening — truly hearing patients without interruption or judgment.
- Non-judgmental language — using words that avoid blame or stigma.
- Consent-based care — making sure patients feel in control of their treatment choices.
Trauma therapy techniques like EMDR (Eye Movement Desensitization and Reprocessing) and CBT (Cognitive Behavioral Therapy) are often part of this care. These methods help address trauma safely and effectively. By receiving trauma-informed training, care teams consistently use these practices to meet patients’ unique needs, focusing on healing rather than just symptoms.
What Is A Trauma-Informed Approach To Treatment?
A trauma-informed approach recognizes how trauma affects a person’s experience of care. It prioritizes emotional safety, trust, and empowerment, ensuring treatment avoids retraumatization. This approach supports healing by respecting each individual’s story and adapting care to meet their unique needs and pace.
What Are The 5 Principles Of Trauma-Informed Care?
The five key principles are: safety, trustworthiness and transparency, peer support, collaboration and mutuality, and empowerment, voice, and choice.
These guide providers to create safe, respectful, and empowering environments that support healing and reduce the risk of re-traumatization.
What Is An Example Of Trauma-Informed Care?
An example is a therapy session where the provider uses active listening, respects boundaries, asks for consent before discussing difficult topics, and adapts the pace to the client’s comfort level. This creates a safe space where the client feels heard, respected, and in control of their healing process.
What Is The Difference Between Trauma Therapy And Trauma-Informed Care?
Trauma therapy is a specific treatment that helps process trauma symptoms, often using methods like EMDR or CBT. Trauma-informed care is a broader approach applied across all services that recognizes trauma’s impact and ensures safety and empowerment, even when trauma therapy is not the main focus.
Taking The Next Step Toward Healing
Healing from trauma is a personal journey, and it’s okay if you don’t have all the answers right now. Trauma-informed care respects your unique story and supports you with choices based on trust and empowerment. This approach creates a safe space where you can move forward at your own pace, feeling seen and understood.
Remember, seeking help is a brave step toward lasting healing. When you’re ready, reaching out to trauma-informed providers can open doors to compassionate support tailored just for you.
Start Your Journey Toward Healing At Rock View Recovery
Rock View Recovery is a premier adult drug and alcohol treatment facility in Arizona that offers compassionate, trauma-informed care. This approach provides a healing path built on safety, trust, and empowerment. Trauma therapy here supports sustainable recovery by honoring your story and meeting you where you are.
You don’t have to face this journey alone. Explore your care options or connect with us today to begin a hopeful, empowering chapter toward lasting healing. Learn more about trauma therapy at Rock View Recovery, or call us at 602-483-6809.
